Background:
The prothrombin time (PT) and activated partial thromboplastin time (aPTT) are often considered “routine” tests to assess perioperative bleeding risk. The PT and its mathematical derivative, the international normalized ratio (INR), allows for monitoring of vitamin K antagonist therapy. The aPTT was developed to screen for hemophilia A and B in family members of affected individuals. Both tests perform extremely poorly as screening tests for inherited bleeding disorders. Therefore, their utility in predicting peri-operative bleeding has been questioned.
Objective:
The primary objective was to examine the relationship between pre-operative coagulation results and peri-operative bleeding in pediatric and adult patients undergoing elective surgery in the published literature.
Methods:
A systematic review was conducted using a comprehensive search of MEDLINE, EMBASE, and grey literature between 1970 to July 2022. Randomized trials and observational studies that assessed the predictive accuracy of pre-procedural INR and aPTT test results for perioperative bleeding we deemed eligible for inclusion. Two reviewers independently screened and performed data extraction. A third reviewer adjudicated decisions when consensus could not be reached. Outcomes included any bleeding events in the postoperative period.
The study protocol was registered online on PROSPERO (CRD42023385588).
Results:
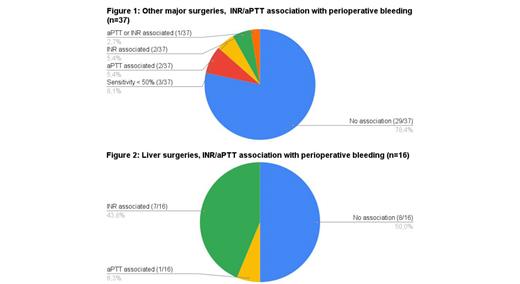
5700 articles were screened, and 79 studies were included in the systematic review. Major surgery (N=53) types included cardiac (n=14), neurosurgery (n=11), liver transplantation or resection (n=16) and general surgery (n=12). Minor surgeries included otolaryngology procedures (n=14) and other minor surgeries/procedures (e.g. pediatric spinal anesthesia, gastrointestinal endoscopy and related procedures, thoracocentesis, hernia repair, circumcision) (n=12). Bleeding complications were rare for minor surgeries and only one out of 26 studies found an association between coagulation test results and bleeding. Thirty-two out of 37 (86.5%) papers exploring other major surgeries found no association or reported a sensitivity under 50% between coagulation test results and bleeding (see Figure 1). Seven out of 16 studies (43.8%) on liver transplantation or resection found an association between the INR and bleeding (see Figure 2). None of the studies evaluated were randomized and none of the observational studies had outcomes adjudicated in blinded fashion.
Conclusion:
Our findings confirm that bleeding events are rare in minor surgeries, and that coagulation testing is of limited utility in this setting. Similar conclusions can be drawn for patients undergoing major surgeries, with one exception - in patients with liver disease or liver cancer - as there may be an association between bleeding and the pre-operative INR with further studies required. Despite the absence of evidence supporting the practice, routine pre-operative coagulation testing remains prevalent, highlighting the need for targeted knowledge translation.
Disclosures
Fralick:Signal1: Membership on an entity's Board of Directors or advisory committees; ProofDx: Consultancy. Sholzberg:Pfizer: Honoraria, Research Funding; CSL Behring: Research Funding; Octapharma: Honoraria, Research Funding.